Alpha gal symptoms

Alpha-gal Syndrome: How a tick bite can trigger a meat allergy
When most people think of food allergies, they imagine having a reaction to peanuts, shellfish, or dairy products. But there’s another type of allergy emerging in certain parts of the United States – and it all starts with a tick bite.
Alpha-gal syndrome (AGS), also known as the red meat allergy, is a serious, potentially life-threatening allergic condition caused primarily by the bite of a lone star tick. Unlike other food allergies, alpha gal symptoms may not appear right away. Symptoms often show up several hours after eating red meat or any foods from mammals, making it difficult to recognize food as the cause.



Alpha-gal Syndrome: How a tick bite can trigger a meat allergy
When most people think of food allergies, they imagine having a reaction to peanuts, shellfish, or dairy products. But there’s another type of allergy emerging in certain parts of the United States – and it all starts with a tick bite.
Alpha-gal syndrome (AGS), also known as the red meat allergy, is a serious, potentially life-threatening allergic condition caused primarily by the bite of a lone star tick. Unlike other food allergies, alpha gal symptoms may not appear right away. Symptoms often show up several hours after eating red meat or any foods from mammals, making it difficult to recognize food as the cause.
What is Alpha-gal?
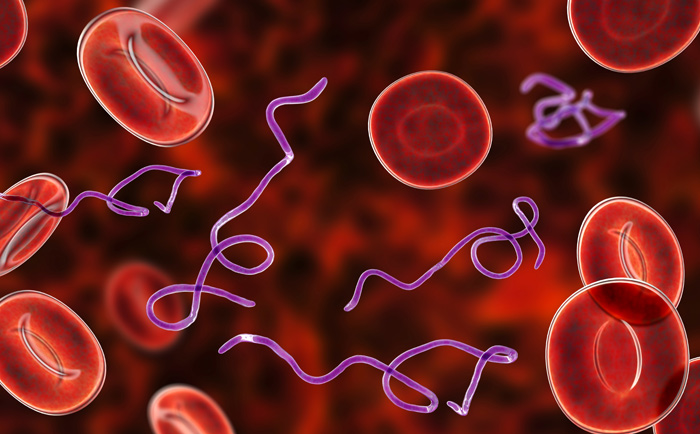
Alpha-gal is a sugar molecule found in most mammals but not in humans. It’s present in foods like beef, pork, lamb, venison, and some dairy products. It is also found in the saliva of some ticks.
Alpha-gal syndrome is caused by a tick bite, primarily from the lone star tick in the U.S. However, it has also been linked to tick bites from the blacklegged tick and western blacklegged tick. In other countries, various tick species can cause AGS.
Alpha-gal is a sugar molecule found in most mammals but not in humans. It’s present in foods like beef, pork, lamb, venison, and some dairy products. It is also found in the saliva of some ticks.
Alpha-gal syndrome is caused by a tick bite, primarily from the lone star tick in the U.S. However, it has also been linked to tick bites from the blacklegged tick and western blacklegged tick. In other countries, various tick species can cause AGS.
What is Alpha-gal?
Alpha-gal is a sugar molecule found in most mammals but not in humans. It’s present in foods like beef, pork, lamb, venison, and some dairy products. It is also found in the saliva of some ticks.
Alpha-gal syndrome is caused by a tick bite, primarily from the lone star tick in the U.S. However, it has also been linked to tick bites from the blacklegged tick and western blacklegged tick. In other countries, various tick species can cause AGS.
When a tick bites, it can pass alpha-gal from its saliva into the bloodstream.
In some people, alpha-gal triggers a reaction in their immune system that causes an allergic response whenever they eat red meat, including beef, pork, or lamb, or food products derived from mammals, such as milk and gelatin.
Need subtitle




What triggers Alpha gal symptoms?
While alpha gal symptoms may take several hours to appear, exposure to alpha-gal via inhalation, injected drugs or vaccines can cause an immediate reaction. Personal products that use ingredients containing “hydrolyzed protein” (gelatin), lanolin, glycerin, collagen, or tallow are particularly problematic.
Additional products that can trigger alpha gal symptoms are jello, gelatin capsules, certain medications, pig or cow heart valves, surgical mesh, certain vaccines and unlabeled “natural flavorings” in foods.
Alpha-gal Syndrome: Common Symptoms
Alpha gal symptoms usually don’t appear right away. They typically show up 2 – 6 hours after eating. This delay can make it hard to identify the food as the cause. Alpha-gal can cause mild to severe symptoms. It also can cause you to have reactions to other foods that come from mammals, such as dairy products or gelatin.
Alpha gal symptoms include:
-
Hives or itchy rash
-
Swelling of lips, face, tongue, or throat
-
Stomach pain, diarrhea, nausea, or vomiting
-
Shortness of breath or wheezing
-
In severe cases, anaphylaxis. This is a potentially life-threatening allergic reaction where blood pressure drops dangerously low and breathing becomes difficult.
Because alpha gal symptoms can appear in the middle of the night (long after dinner), people may not immediately suspect a food allergy. In fact, researchers believe that some individuals may have alpha-gal syndrome and not even know it.
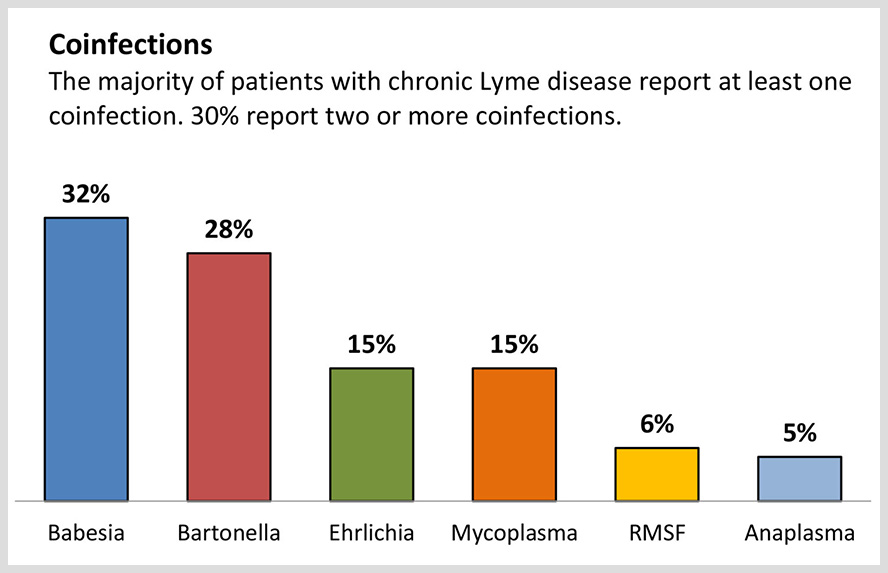
Top Co-Infections in Lyme Disease Patients
According to a survey by Lymedisease.org, out of 3,000 patients with chronic Lyme disease, over 50% had co-infections, with 30% reporting 2 or more. The most common Lyme disease coinfections include: Babesiosis (32%), Bartonella (28%), Ehrlichia (15%), Mycoplasma (15%), Rocky Mountain spotted fever (6%), and Anaplasma (5%).
How Common Are Co-Infections?
In the northeastern U.S., studies have found that up to 45% of blacklegged ticks carry more than one pathogen ─ meaning that a single tick bite can result in co-infections. And, up to a third of individuals diagnosed with Lyme disease, may also have at least one co-infection.
A survey conducted in endemic regions reported that nearly 1 in 5 people with Lyme disease also tested positive for the co-infection babesiosis.

However, in a study by Sperling and colleagues, the most common coinfections found in patients with Lyme disease were Bartonella (36%) and Babesia (19%), followed by Anaplasma (13%). The specific co-infections people develop can vary depending on geography. In this case, the study involved primarily Canadian patients.
Note: While both ticks and humans are known to carry Bartonella, scientists are still studying the exact way this infection is transmitted.
While anaplasmosis and ehrlichiosis are less common, they still impact up to 10% of Lyme patients. And recent data indicates that the number of cases of Borrelia miyamotoi, another coinfection, is on the rise.
Note: The information presented on this page has been reviewed and approved by a member of our Medical Leadership Board.
Could your symptoms be due to a tick-borne disease infection?
Take the first step towards understanding tick-borne disease with an exclusive guide to something here, all backed by world-leading science.
More Lyme Basics
Join Our
Newsletter
A short introduction to why to join newsletter
Join our Newsletter
If you or a loved one has been affected by Lyme disease, we have resources and news to help guide you through your experience and keep you updated on important news stories about Lyme disease.

Sample Subtitle
Modi temora incidunt ut labor magna!
Sed ut unde omnis iste natus sit volur tatem accus antium laudan tium totam rem aperiam eaque ipsa ab illo inventore veritatis et architecto beatae vitae dicta sunt explicabo.