Bartonella Treatment

Why Bartonella Treatment Is So Complex
Bartonella treatment and diagnosis can be complex because the bacteria are hard to detect and difficult to eliminate. They hide inside red blood cells and blood-vessel walls, often causing vague or overlapping symptoms that mimic other infections. Accurate diagnosis requires specialized testing, and Bartonella treatment typically involves targeted antibiotics and careful medical monitoring to ensure full recovery.
Bartonella: A challenging diagnosis
Bartonella is diagnosed based on a patient’s symptoms, physical examination, medical history and laboratory testing for confirmation. Identifying Bartonella through testing can be extremely difficult because the bacteria hide inside red blood cells and the lining of blood vessels. This allows them to evade detection by the immune system and makes standard laboratory tests less reliable. Because diagnosis can be challenging, Bartonella treatment often depends on clinical judgement.
However, several tests are available. Indirect immunofluorescence assay (IFA) can detect antibodies against Bartonella in the blood but only for a few Bartonella species.
While the test is considered highly insensitive, IFA testing can provide evidence of exposure but it cannot confirm an active infection. Other tests include polymerase chain reaction (PCR), fluorescent in situ hybridization (FISH) and blood cultures.
Specialty laboratories have developed advanced methods to improve detection of Bartonella. Galaxy Diagnostics offers a combination of culture and PCR testing, known as ePCR, which is designed to more effectively identify active infection. Similarly, IGeneX provides a CultureEnhanced PCR (cePCR) test that uses a comparable approach to increase the likelihood of detecting the bacteria.
Bartonella Treatment Options
Since the infection can affect many different systems in the body, Bartonella treatment often needs to be tailored to the individual and the severity of their infection. And, because symptoms can mimic many other conditions, professional evaluation is essential to determine whether Bartonella treatment is needed.
Bartonella treatment typically involves the use of antibiotics. The choice of medication may vary depending on the specific Bartonella species involved, the patient’s age, medical history, and the severity of illness.
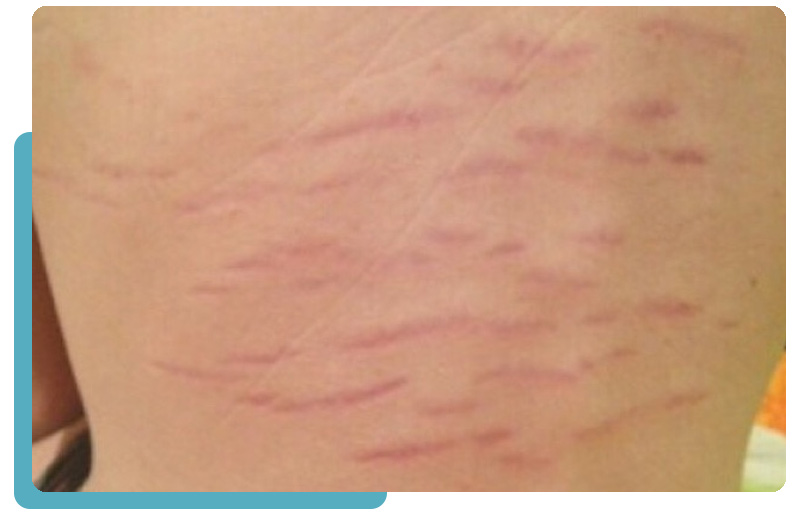
For mild cases, the infection may resolve on its own, but antibiotics are sometimes prescribed to speed recovery or reduce complications. More complex or chronic Bartonella infections, including those affecting the nervous system, may require longer or a combination of antibiotic treatment. Because Bartonella bacteria live inside red blood cells and blood vessel linings, the infection can be difficult to completely eliminate, making persistence or relapse possible. This is why treatment plans often include follow-up testing, supportive care for symptoms, and in some cases, management of other coinfections.
Bartonella Treatment: FAQ
Note: The information presented on this page has been reviewed and approved by a member of our Medical Leadership Board.
Could your symptoms be due to a tick-borne disease infection?
Take the first step towards understanding tick-borne disease with an exclusive guide to something here, all backed by world-leading science.